In this video I address the issue of what you need to know about the therapeutic care and management of children and young people diagnosed with ASD and/or ADHD, where there is a trauma overlay. The video is intended to be of most interest to those who interact with children and young people who are recovering from a tough start to life in care and professional roles.
Disclaimer: While great care is taken to ensure that the information in this audio/video is applicable to childhood trauma and based on sound psychological science, it may not suit the individual circumstances of all viewers. If you have any concerns about applicability to your circumstances, please consult a qualified professional near to you.
Transcript:
Just on the issue of children being diagnosed with Attention Deficit Hyperactivity Disorder and or Autism Spectrum Disorder, where these children also they’re in a statutory kinship care placement, so there’s been some concerns that have meant that they couldn’t safely be cared for at home with their mum and or their dad, so they’re living with other family and so that creates another layer to their experience. Okay, so in the out-of-home care space, though a child or young person may be diagnosed with Autism Spectrum Disorder or Attention Deficit Hyperactivity Disorder or both, there is also a trauma overlay which derives from their prior experience when they could not be safely cared for at home with mum and or dad and I believe this also applies to children who are removed at birth. Their trauma derives from antenatal factors but more importantly, I think, from their experience and the meaning they make of not being able to live with mum and or dad.
Anyway, it’s important to recognise and acknowledge the trauma overlay because it influences how we work with these children and young people, especially in consideration that a trauma-informed approach, which is necessary when there is a trauma overlay, requires us to look beyond the presenting behaviours of concern and to respond therapeutically to the reasons for them. This is highlighted in this slide. I’ve chosen a number of common behaviours of concern here and as you can see, it is my contention that we see these behaviours, whether the child is diagnosed with a neurodevelopmental disorder like ASD or ADHD or has a history of developmental trauma.
In fact, I could add a fourth column, one for children and young people who have no diagnosis or trauma history. They exhibit these behaviours too. However, there are two further considerations here.
One, that normality and abnormality are differentiated by frequency, intensity and duration. So, kids with ASD or ADHD and a trauma history exhibit these behaviours at a greater frequency, intensity and duration such that it impacts adversely on their approach to life and relationships. The second consideration has to do with the reasons why these behaviours occur that are often different for ASD versus ADHD versus trauma.
If the reason for the behaviour is different, our approach to responding therapeutically to them is often different. This is reflected in this slide where I present the reasons why we see these behaviours in children with ASD, ADHD and those who have experienced developmental trauma. As you can see, there are similarities and differences.
If we are to respond therapeutically to the behaviour, we need to address all of the reasons for it. Which brings me to this slide. In this slide, I present what a therapeutic response looks like for each of the reasons for these common behaviours.
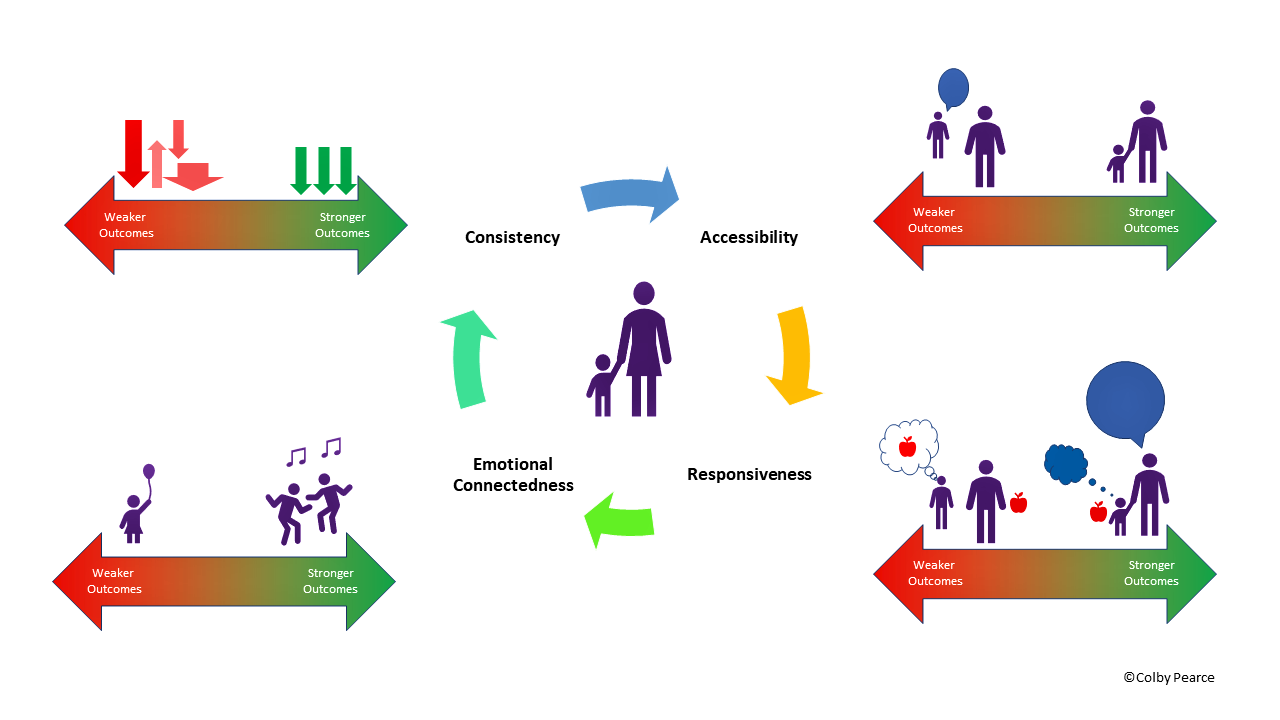
As you can see, there are similarities and differences. This seems quite complex until we map the care model onto the same slide. Where care involves enriching a child’s experience of consistency, the accessibility of adults in their life who have a caring concern for them, the responsiveness of those adults and the emotional connectedness of those adults. When we map the care model onto these reasons, for each of these behaviours that we see in autism spectrum disorder, attention deficit hyperactivity disorder and or where there is a history of developmental trauma, there is a care strategy to address the reasons for the behaviour, notwithstanding diagnosis or trauma history.